What is Gamma Knife radiosurgery?
Gamma Knife radiosurgery, also called stereotactic radiosurgery, is a very precise form of therapeutic radiology.
Even though it is called surgery, a Gamma Knife procedure does not involve actual surgery, nor is the Gamma Knife really a knife at all. It uses beams of highly-focused gamma rays to treat small to medium size lesions, usually in the brain.
Many beams of gamma radiation join to focus on the lesion under treatment, providing a very intense dose of radiation without a surgical incision or opening.
Gamma Knife radiosurgery is called “surgery” because a result similar to an actual surgical procedure is created by a one-session radiation therapy treatment. The beams of radiation are very precisely focused to reach the tumor, lesion, or other area being treated with minimal effect on surrounding healthy tissue.
Gamma Knife radiosurgery is most often used to treat
- tumors and other lesions in the brain.
It is also used to treat certain neurological conditions, such as
- trigeminal neuralgia (a condition in which pressure on the trigeminal nerve causes spasms of extreme facial pain)
- acoustic neuroma (a noncancerous tumor in the brain that affects the nerves that control hearing).
Gamma Knife radiosurgery may be used in situations where the brain lesion cannot be reached by conventional surgical techniques. It may also be used in persons whose condition is such that they might not be able to tolerate a surgical procedure, such as craniotomy, to treat their condition.
Because the therapeutic effects of a Gamma Knife procedure occur rather slowly over time, it is NOT used for cases in which a more immediate therapy is required.
How does Gamma Knife radiosurgery work?
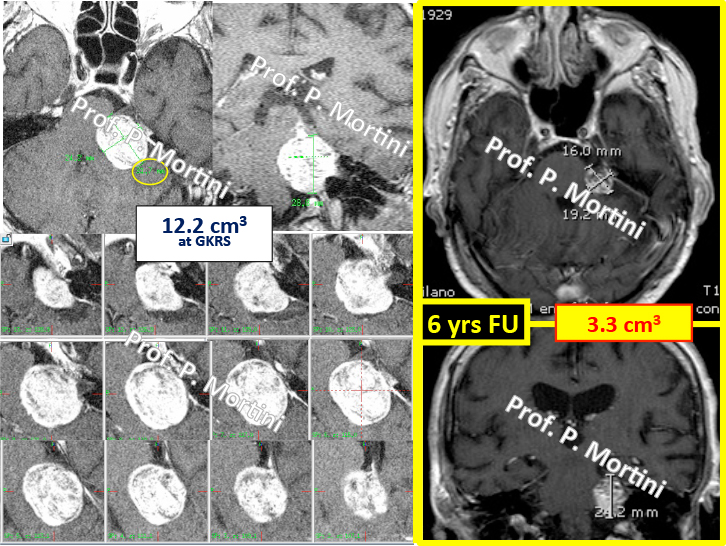
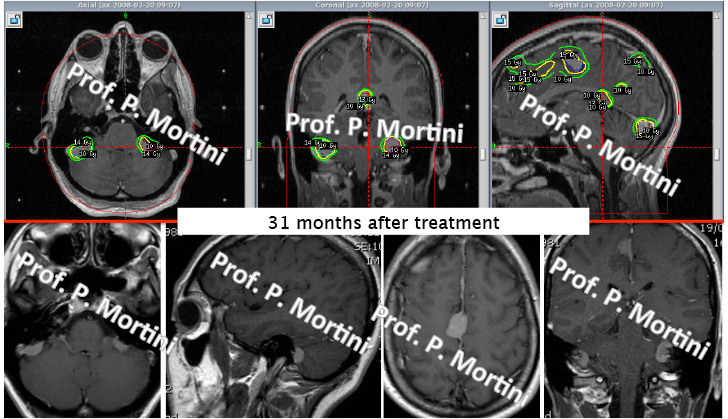
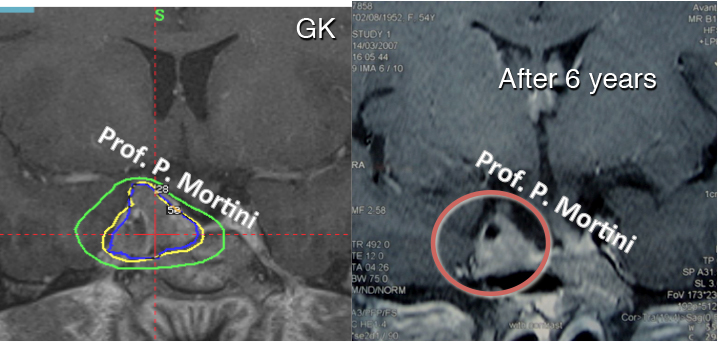
Radiosurgery works in the same manner as other types of therapeutic radiology: it distorts or destroys the DNA of tumor cells, causing them to be unable to reproduce and grow. The tumor will shrink in size over time.
For blood vessel lesions such as an Arteriovenous Malformation (AVM), the blood vessels eventually close off after treatment.
Gamma Knife treatment generally involves these steps:
1 – head frame placement
In order to keep the head from moving during treatment, a box-shaped frame is attached to the head. Pins designed specifically for this purpose fasten the head frame to the skull. The head frame also is a guide to focus the gamma ray beams to the exact location of the lesion being treated.
2 – tumor or lesion location imaging
Once the head frame is in place, the exact location of the lesion to be treated will be determined using computed tomography (CT scan) or magnetic resonance imaging (MRI).
3 – radiation dose planning
After the CT or MRI scan has been completed, the radiation therapy team will determine the treatment plan. The results of the imaging scan, along with other information, will be used by a medical physicist to determine the best treatment.
4 – radiation treatment
After being positioned for the treatment, a type of helmet with many hundreds of holes in it is placed over the head frame. These holes help to focus the radiation beams on the target. Treatment will last a few minutes up to a few hours, depending on the type and location of the area being treated. Generally, only one treatment session is required for a lesion.
A Gamma Knife procedure involves a treatment team approach. The treatment team generally includes a radiation oncologist (a physician specializing in radiation treatment for cancer), a neurosurgeon and/or a neuroradiologist, a radiation therapist, and the nurse staff.
In addition, a medical physicist and a dosimetrist work together to calculate the precise number of exposures and beam placement necessary to obtain the radiation dose that is prescribed by the radiation oncologist.
The Gamma Knife system is one of three types of radiosurgery systems. Two other types of radiosurgery are linear accelerator (LINAC) systems and proton beam therapy or cyclotron.
Reasons for the Procedure
Gamma Knife radiosurgery may be used to treat certain conditions of the brain in particular instances. Brain conditions that may be treated with a Gamma Knife procedure include, but are not limited to, the following:
• brain tumors
• brain cancer
• arteriovenous malformations, or AVM (a type of blood vessel defect)
• trigeminal neuralgia
• acoustic neuroma
Gamma Knife radiosurgery has shown some promise for treating conditions such as tremor and rigidity related to Parkinson’s disease, and epilepsy.
Risks of the Procedure
If you are pregnant or suspect that you may be pregnant, you should notify your physician. Radiation exposure during pregnancy may lead to birth defects.
Other risks and side effects (that may also depend upon your specific medical condition) will be explained by the neurosurgeon during the preliminary visit that is necessary for evaluation.
Before the Procedure
• Your physician will explain the procedure to you and offer you the opportunity to ask any questions that you might have about the procedure.
• You will be asked to sign a consent form that gives your permission to do the procedure. Read the form carefully and ask questions if something is not clear.
• In addition to a complete medical history, your physician may perform a complete physical examination to ensure you are in good health before undergoing the procedure. You may undergo blood tests or other diagnostic tests.
• Notify your physician if you are sensitive to or are allergic to any
- medications
- latex
- tape
- contrast dyes
- iodine
- shellfish
- anesthetic agents (local and general).
Notify your physician:
– of all medications and supplements that you are taking
– if you have a history of bleeding disorders or if you are taking any anticoagulant (blood-thinning) medications, aspirin, or other medications that affect blood clotting
– if you have any type of implant(s), such as a pacemaker and/or implantable defibrillator, artificial heart valve, surgical clips for a brain aneurysm, implanted medications pump, chemotherapy port, nerve stimulators, eye or ear implants, stents, coils, or filters.
– Ii you are pregnant or suspect that you are pregnant
Doctors will provide you details on preparation, pre-treatment and post-treatment procedures.
During the Procedure
Generally, a Gamma Knife procedure follows this process:
1. You will be asked to remove any clothing, jewelry, hairpins, dentures, or other objects that may interfere with the procedure, and will be given a gown to wear.
2. An intravenous (IV) line may be started to give medications and/or fluids during the procedure.
3. The skin on your head will be cleansed at the locations where the pins for the head frame will be placed.
4. A local anesthetic will be injected at the head frame pin insertion sites. Once the anesthetic has taken effect, the head frame will be attached to your head with pins that are inserted into your skull.
5. After the head frame is attached, you will undergo brain imaging as a computed tomography (CT) scan, a magnetic resonance imaging (MRI) scan, or a cerebral angiogram.
7. After the brain imaging has been completed, you will be allowed to rest and relax while the treatment team completes your treatment plan.
8. When your treatment plan is ready, you will lie down on a sliding table of the Gamma Knife machine and a collimator helmet will be fitted over the head frame.
9. Once the helmet is in place, the table will slide into the Gamma Knife unit and the treatment will start.
10. The number and lenghts of treatment/s will depend on your specific situation and will be discussed with the doctors.
12. You will not feel or hear anything from the Gamma Knife unit during the treatment session. The treatment is not painful.
After the Procedure
You may feel some discomfort after the procedure, such as a headache or nausea or other sympthoms that will be explained in details by your doctor.
 English
English Italiano
Italiano